In reaction to the tumult over high insulin prices, the Food and Drug Administration (FDA) has been firming up its plans for a transition to biosimilar competition for insulin. Lilly, one of the dominant insulin manufacturers in the US, has decided to cut prices through the authorized generic route.
In this case, a manufacturer that owns a branded product with expiring patents may decide to get the upper hand on the impending competition by launching its own low-cost generic version well before other agents can be marketed. With a so-called authorized generic, the drug company may produce the new version itself or sign a royalty agreement with another manufacturer to secure a share of the profits.
The FDA wants to encourage the entry of new competitive players into the insulin arena to lower costs. However, the first entrants (for insulin glargine) were follow-on biologics, not biosimilars. Follow-on insulins are currently regulated under section 505b2 of the Food, Drug, and Cosmetics Act (which covers small molecules and early biologic compounds), not section 351 of the Public Health Service Act (which covers biologics and biosimilars). The transition to regulation under the Public Health Act is not expected to begin until March 2020.
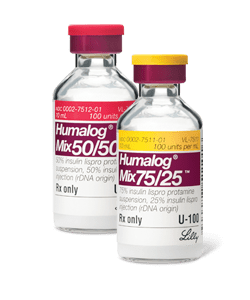
Eli Lilly announced on March 4 that it will sell Humalog® (insulin lispro) as an authorized generic. The Humalog authorized generic will be sold at a 50% discount to the brand’s wholesale acquisition cost. It will be distributed through its ImClone Systems subsidiary. This does not mean that Humalog will no longer be sold. Instead, it will continue to offer the branded version at its same price (and rebates) to payers who prefer this arrangement. Instead, the authorized generic will be sold directly to patients or others who do not benefit from the rebate revenue.
Lilly stated that the new generic version will be available “as soon as possible.” Some believe that a 50% discount is only a half-step. At $137.35 per vial, it is difficult to believe that a patient with a drug deductible or who is uninsured can easily pay the monthly cost of insulin treatment. Brand manufacturers can partly deflect scrutiny through such actions. However, with the prices of several older and brand new categories of drugs considered too high, pressure will remain on drug makers, law makers, and regulators to further lower costs.
In related biosimilar news…Four US Senators have sent a letter to the FDA to ensure that the transition period does not slow competition for insulin products. One aspect of this was the potential need for prospective makers of 505b2 insulins to have to resubmit their drug applications under the 351(k) biosimilar provisions. This could significantly delay entry into the market.

 the application itself.
the application itself.