AbbVie executives are sticking to their pledge to restrict annual price increases on Humira® below 10%, but even payer price protections won’t mitigate the increasing expenditures before adalimumab biosimilars hit the market. In 2023, when adalimumab biosimilars become available, the savings biosimilars represent may not be real savings at all.
Pharmaceutical companies generally seek to lock in preferred coverage status for their agents through the use of rebates, which lowers the net costs. Typical in these contracts is a price guarantee, which shields the payer from annual (or more frequent) price increases for the duration of the contract. The contract life is one or two years, after which the health plan, insurer, health system, or pharmacy benefits manager must renegotiate—that means significantly higher costs for each successive contract renewal.
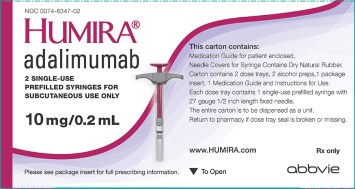
Drug price increases for self-injectable medications like adalimumab, are reported on top of its wholesale acquisition cost (WAC), or the list price. Rebates are applied to WAC pricing. Therefore, if for example, a manufacturer announces 9% price increase to drug X, that applies to the WAC price and does not include consideration of rebates or price guarantees secured by a payer. Rebate information is notoriously difficult to obtain, as payers and pharmaceutical companies consider them proprietary.
However, in a January piece in the New York Times, the author cites research by SSR Health, which concludes that the price of Humira with rebates rose 100% since 2012 to an average of approximately $38,000. Assuming AbbVie executives hold to their price increase pledge, raising their prices by only 6% per year, by 2023 when patent expirations will bring a rash of biosimilars to market, Humira’s price after rebates would have risen 33.8%, to $50,844. If the price is jacked up 9% per year, that would be an increase of 53.9%, to $58,482. This is assuming of course that AbbVie does not increase the rebate at each contract negotiation to offset the higher net cost. To make this dystopian vision complete, let’s not forget that the full savings will not obtained over a population unless all utilization is fully converted to a biosimilar from Humira. That may require an interchangeable biosimilar product (which has not yet been approved) .
As we reported last year, the Institute for Cost-Effectiveness Research established that to meet accepted thresholds for cost-effectiveness, Humira would have to be discounted 55% from its list price. Rises in the cost-effectiveness thresholds (currently $100,000–150,000 per quality-adjusted life-year) would never keep up with this pace of price increases. By 2023, Humira will be even further off the mark in terms of providing value.
The most important point of this, is that the cost savings of the biosimilars that are finally introduced could be an illusion. If a price war in 2023 for newly available adalimumab biosimilars results in 50% discounts, we may have received little but a roll back in costs to those of today. From the perspective of 2018, that’s not savings. That is price stability.
I wrote in 2016 of the same effect for Enbrel®. Because Amgen had taken multiple price increases in the previous years, the WAC cost jumped 37%. And in 2018, no biosimilar is presently marketed for prescription in the United States. The relative discount by Sandoz (presently the sole US company with an approved biosimilar etanercept) needed to actually save payers money for etanercept will not be realistic.
